Breast cancer is a critical health issue that impacts millions globally, including both women and men. Gaining a deeper understanding of this disease—its stages, symptoms, and treatment options—empowers individuals to take proactive measures for early detection and effective intervention. We explores the vital aspects of breast cancer, offering clear and concise information to help everyone stay informed and prepared. Whether you are seeking to educate yourself or support a loved one, this guide aims to provide the knowledge you need to navigate the complexities of breast cancer with confidence and hope.

Breast cancer begins when cells in the breast start to grow uncontrollably. These cells usually form a tumor that can often be seen on an X-ray or felt as a lump. Breast cancer occurs mostly in women, but men can get breast cancer too. There are different types of breast cancer, depending on which cells in the breast turn into cancer. Most breast cancers are carcinomas, which are tumors that start in the epithelial cells lining organs and tissues. Breast cancer can start in different parts of the breast, such as the ducts, the lobules, or in some cases, the tissue in between.
How Many Stages of Breast Cancer Are There?
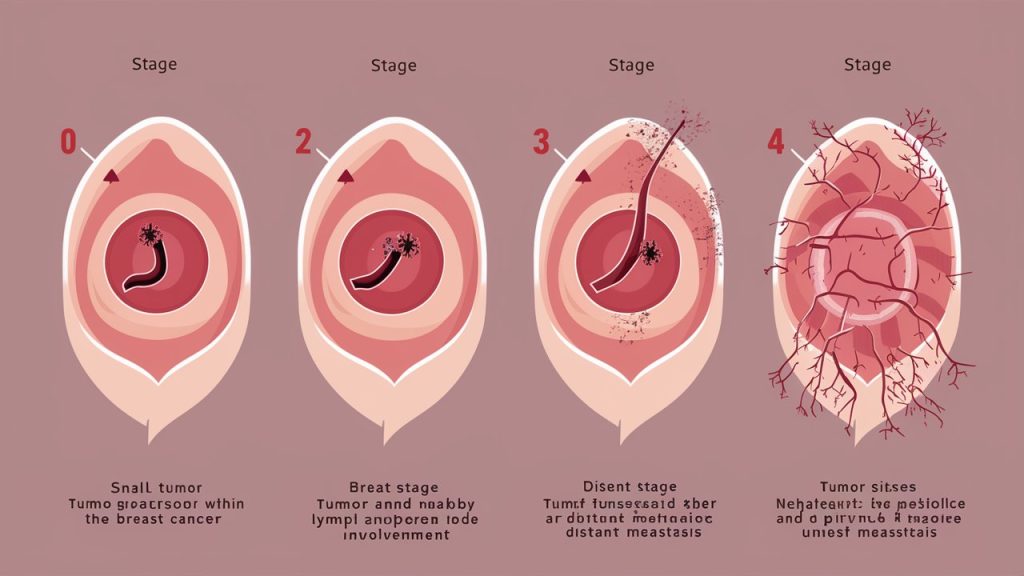
Breast cancer is categorized into stages based on the size of the tumor and the extent to which it has spread. There are five main stages:
- Stage 0: Known as ductal carcinoma in situ (DCIS), where cancer cells are confined within the ducts and have not spread to surrounding tissues. This stage is considered non-invasive, meaning it hasn’t invaded nearby tissue.
- Stage 1:
- Stage 1A: Tumor is up to 2 cm and hasn’t spread outside the breast. This is the earliest stage of invasive breast cancer.
- Stage 1B: Small clusters of cancer cells are found in lymph nodes and either no tumor in the breast or a tumor smaller than 2 cm. This indicates that the cancer has begun to spread outside the ducts but is still quite small.
- Stage 2:
- Stage 2A: Tumor is 2-5 cm, or cancer has spread to 1-3 nearby lymph nodes. This stage may also include tumors larger than 5 cm that have not spread to any lymph nodes.
- Stage 2B: Tumor is larger than 5 cm but hasn’t spread to lymph nodes. This indicates more advanced local disease but still confined within the breast or nearby lymph nodes.
- Stage 3:
- Stage 3A: Tumor up to 5 cm and spread to 4-9 lymph nodes or larger than 5 cm with small clusters of cancer cells in lymph nodes. This stage is more extensive within the regional area.
- Stage 3B: Tumor has spread to the chest wall or skin and up to 9 lymph nodes. This stage indicates more serious local invasion.
- Stage 3C: Cancer in 10 or more lymph nodes, lymph nodes above or below the collarbone, or nearby tissues. This is a very advanced local or regional disease.
- Stage 4: Known as metastatic breast cancer, where cancer has spread to other parts of the body, such as bones, liver, lungs, or brain. This stage indicates that the cancer has spread beyond the breast and nearby lymph nodes to other organs.
How to Detect Breast Cancer?
Early detection of breast cancer can significantly increase the chances of successful treatment. Common methods include self-examination, clinical examination, mammography, ultrasound, and MRI.

- Self-Examination: Regularly checking your breasts for any lumps, changes in size, shape, or skin texture is crucial. This should be done monthly. Look for any discharge from the nipples, dimpling of the skin, or changes in nipple appearance. While self-exams are not a substitute for professional screenings, they can help you become familiar with your breasts and notice any changes earlier.
- Clinical Examination: A doctor or nurse checks for lumps or other changes in the breasts during a physical exam. This is recommended annually for women over 40 but can be beneficial for younger women with high risk. The healthcare provider will use their hands to feel for lumps or abnormalities in the breast tissue and underarms.
- Mammography: An X-ray of the breast used to detect tumors that cannot be felt. Recommended every 1-2 years for women aged 50-74. Women at higher risk may start earlier. Mammograms can detect tumors that are too small to be felt and can identify micro calcifications that sometimes indicate the presence of breast cancer.
- Ultrasound: Uses sound waves to create images of breast tissue. Often used alongside mammography, especially in women with dense breast tissue. Ultrasound can help differentiate between solid masses and fluid-filled cysts and can provide a clearer picture in dense breast tissue where mammography might not be as effective.
- MRI: Magnetic Resonance Imaging for detailed images. Used for high-risk patients, MRI is more sensitive than mammography and can detect tumors that mammograms might miss. It’s particularly useful for women with a high genetic risk or those with dense breast tissue.
What Are the Treatments for Breast Cancer?
The treatment plan for breast cancer depends on its stage, type, and individual patient factors. Common treatments include surgery, radiation therapy, chemotherapy, hormone therapy, and targeted therapy.
- Surgery: Surgical options are often the first line of treatment for breast cancer.
- Lumpectomy: This procedure involves removing the tumor and a small margin of surrounding tissue. It’s often referred to as breast-conserving surgery because it leaves most of the breast intact.
- Mastectomy: This involves removing one or both breasts, partially or completely. There are different types of mastectomies, including total (simple) mastectomy and modified radical mastectomy.
- Radiation Therapy: High-energy waves are used to kill cancer cells. Radiation is often used after surgery to eliminate any remaining cancer cells in the breast, chest wall, or axillary (underarm) lymph nodes. It can be administered externally or internally (brachytherapy).
- Chemotherapy: Chemotherapy uses drugs to kill cancer cells or stop their growth. This can be given before surgery (neoadjuvant chemotherapy) to shrink tumors or after surgery (adjuvant chemotherapy) to prevent recurrence. Chemotherapy is also used in advanced breast cancer to control the disease and prolong life.
- Hormone Therapy: Used for cancers that are hormone receptor-positive, hormone therapy blocks the body’s natural hormones that fuel cancer growth. Drugs like tamoxifen or aromatase inhibitors are commonly used. Hormone therapy can be effective in reducing the risk of cancer recurrence and in treating metastatic cancer.
- Targeted Therapy: Drugs that specifically target cancer cells without affecting normal cells. Example: HER2 inhibitors for HER2-positive breast cancer, such as trastuzumab (Herceptin). Targeted therapies are designed to attack specific genetic mutations or proteins that contribute to cancer growth.
What Are the Causes and Risk Factors of Breast Cancer?
Several factors can increase the risk of developing breast cancer, though having one or more risk factors does not mean you will get the disease. Common risk factors include genetic factors, family history, age, hormonal factors, and lifestyle factors.
- Genetic Factors: Mutations in genes like BRCA1 and BRCA2 can significantly increase the risk of breast cancer. Women with these genetic mutations have a higher likelihood of developing breast and ovarian cancers.
- Family History: Having close relatives with breast cancer increases your risk. If your mother, sister, or daughter has been diagnosed with breast cancer, especially at a young age, your risk is higher.
- Age: Risk increases with age, especially after 50. Most breast cancers are diagnosed in women over the age of 55.
- Hormonal Factors: Early menstruation (before age 12) or late menopause (after age 55) can increase the risk due to longer lifetime exposure to estrogen and progesterone. Hormone replacement therapy during menopause, especially combined hormone therapy, also raises the risk.
- Lifestyle Factors:
- Lack of physical activity: Regular exercise helps maintain a healthy weight and balance hormone levels.
- Poor diet: Diets high in saturated fats and low in fruits and vegetables may increase the risk.
- Alcohol consumption: Drinking alcohol is linked to an increased risk of breast cancer.
- Obesity: Excess body fat, especially after menopause, can increase estrogen levels, contributing to higher breast cancer risk.

Precautions and Preventive Measures
Taking steps to reduce your risk of breast cancer is crucial. Here are some preventive measures:
- Healthy Diet: Eat a balanced diet rich in fruits, vegetables, and whole grains. Limit red meat and processed foods. Foods high in antioxidants, fiber, and healthy fats (like omega-3 fatty acids) can help reduce cancer risk.
- Regular Exercise: Aim for at least 30 minutes of moderate exercise most days of the week. Exercise helps control weight, boosts immune function, and reduces levels of estrogen and insulin.
- Limit Alcohol: Limit intake to one drink per day. Alcohol can increase estrogen levels and potentially damage DNA in cells.
- Avoid Smoking: Smoking is linked to many cancers, including breast cancer. Quitting smoking can significantly reduce your overall cancer risk.
- Regular Screenings: Follow guidelines for mammograms and clinical exams. Early detection through regular screening can help find breast cancer early when it is most treatable.
- Breastfeeding: Breastfeeding for several months may lower the risk. It is thought that breastfeeding may protect against breast cancer by reducing a woman’s total number of menstrual cycles in her lifetime.
Take Charge of Your Breast Health with Dr. Garima
Breast cancer awareness and early detection are essential in the fight against this pervasive disease. Empower yourself with knowledge about the symptoms, stages, and cutting-edge treatments available. Remember, early detection significantly improves the chances of successful treatment and recovery.
Dr. Garima, a leading oncology specialist, is dedicated to providing comprehensive care for those affected by breast cancer. With her expertise and compassionate approach, she guides patients through every step of their journey—from diagnosis to treatment and beyond.
If you want more info, please contact Easytreatmentindia